How long aftee dental implant can i take fosamax
Why do bisphosphonates cause osteonecrosis of the jaw?
Bisphosphonate-related osteonecrosis of the jaw (BRONJ) is thought to cause damage to the dentoalveolar structures that have limited ability to heal bones due to the therapeutic effect of biphosphonate. This may interest you : What is the downside of dental implants?. See below for a picture of the emerging, necrotic bone of the anterior left maxilla.
Why do biphosphonates cause MRONJ? Several studies have suggested that bifosphonates cause excessive bone loss, resulting in a higher risk of bone necrosis when repair is needed. It is also thought that bisfosphonates bind to osteoclasts and interfere with bone remodeling.
What do bisphosphonates do to the bone and why?
Bisphosphonates work by lowering osteoclasts. They therefore reduce bone loss, which allows osteoblasts to function more efficiently. See the article : Does colorado medicaid cover dental implants. They can help strengthen the bones and help prevent it from becoming weaker.
How do bisphosphonates prevent bone loss?
Bisphosphonates reduce the risk of fractures by inhibiting bone resorption and increasing bone strength, and have been widely used in the prevention and treatment of osteoporosis. However, the use of these drugs in the management of osteoporosis remains a health challenge.
How do bisphosphonates affect bone healing?
Conclusion. This meta-analysis showed that bisphosphonate did not significantly affect bone healing time but increased BMD changes and reduced bone resorption and regression symptoms. Applying bisphosphate in the early stages after injury is the right choice for fracture healing.
How do bisphosphonates affect the jaw?
Bisphosphonate-related osteonecrosis of the jaw (BRONJ) is a chronic condition in the oral cavity that results in mucosal ulcers and exposure to the lower necrotic bone, and subsequent complications. This may interest you : How long after flapless dental implant can i smoke?. As a newly identified condition, the BRONJ epidemic has been poorly described.
Does bisphosphonates cause osteonecrosis of jaw?
Recently, however, high doses of infusion bifosphonates have been identified as a risk factor for osteonecrosis of the jaw in cancer patients. Low bisphosphonate use in patients with osteoporosis or other metabolic disorders has not been associated with the development of osteonecrosis of the jaw.
How common is jaw necrosis with bisphosphonates?
Osteoporosis, bisphosphonate-associated osteonecrosis of the jaw is rare, and the incidence is less than natural. Infectious disease research has shown that it is estimated to be less than 1 in 100,000 cases per year of oral bifosphonates.
How common is jaw necrosis with bisphosphonates?
Osteoporosis, bisphosphonate-associated osteonecrosis of the jaw is rare, and the incidence is less than natural. Infectious disease research has shown that it is estimated to be less than 1 in 100,000 cases per year of oral bifosphonates.
How rare is osteonecrosis of the jaw?
We do not know who will develop and who will not. Studies show that about 1% to 2% of people (1 to 2 in 100) who take these anti-cancer drugs will have ONJ. The risk is very low for people taking it to treat osteoporosis.
How common is osteonecrosis of the jaw with Prolia?
In cancer patients exposed to denosumab, the risk of ONJ varies from 0.7 to 1.9% (70 to 90 cases per 10,000 patients).
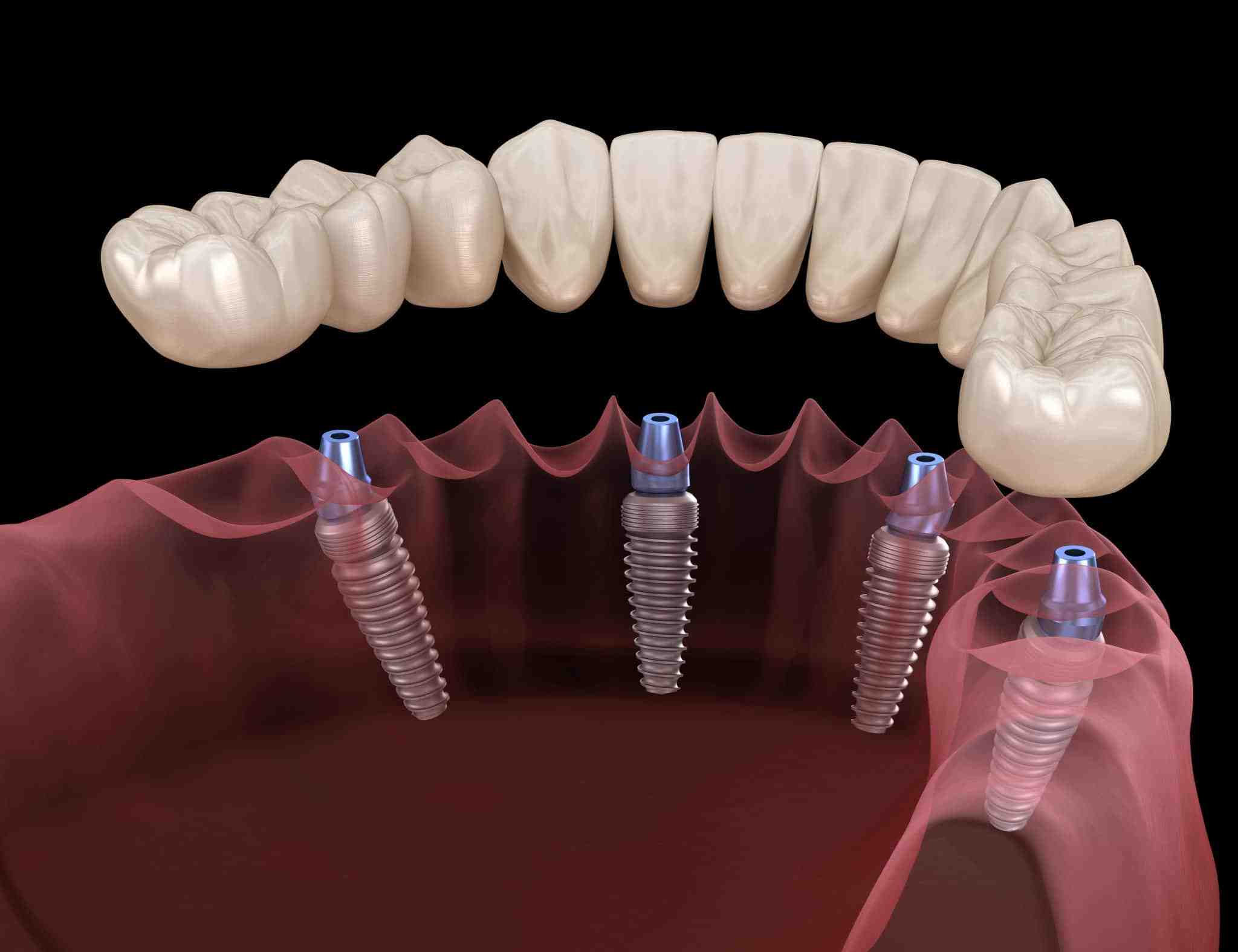
Can I have tooth implant if I have osteoporosis?
The answer is the involvement of the jaw bone and the bones around the face. If the bone marrow volume is affected by the development of osteoporosis, the bone cannot accept the dental vaccine. Permission is important because dental implants fit into your body to provide stability.
Who should not get the dental vaccine? People taking certain medications, such as steroids or drugs that suppress the immune system, may not be the right candidates, either. And people with certain habits, such as those who grind or grind their teeth badly, may put too much pressure on the implant, causing long-term damage.
What if there is not enough bone for dental implants?
If you are told you do not have enough bones to be vaccinated, we may recommend a bone graft or recovery (to create a healthy bone graft), or a free quick fix using a limited bone graft reliable. the method of implantation.
Can you get dental implants if you have bone loss?
Yes, people with severe osteoporosis are eligible for the dental vaccine. In many cases, this can be done without long-term bone grafting procedures. The specialist dentist considers many factors before recommending a dental vaccine solution.
How much bone is needed for a dental implant?
For general instructions, at least 1 mm of bone is needed around the dental implant. More space is needed when the implant is next to a tooth or elsewhere. If there are not enough bones to completely cover the implant, bones will be needed.
How does osteoporosis affect dental treatment?
Osteoporosis affects all bones in the body, including the jawbone. Loss of bone density in the jaw reduces tooth stability, increases the risk of tooth loss and urinary tract infections. Osteoporosis affects the teeth as well as the implanted teeth, and can limit treatment options for your teeth.
Can osteoporosis affect mouth?
Research suggests a link between osteoporosis and jaw bone loss. The bone in the jaw supports and attaches to the teeth. When the jaw bone becomes dense, the tooth may fall out, a common occurrence in adults.
Can a person with osteoporosis get dental implants?
Therefore, osteoporosis is considered a questionable question of tooth placement. However the literature states that patients with osteoporosis do not appear to be at high risk for bone grafting. Patients with osteoporosis are not immune to toothpaste.
Are bisphosphonates a contraindication for implants?
Intravenous administration (IV) of bisphosphonates is considered a complete contraindication for dental placement, due to the increased risk of bisfosphonate-associated bone-osteonecrosis of the jaw (BRONJ).
Does osteoporosis prevent tooth decay? Therefore, orthopedic surgery is not the opposite of implanted surgery because an accurate analysis of bone quality through imaging is performed.
What are some contraindications for dental implants?
Complete challenges for dermatological rehabilitation include myocardial infarction and brain accidents, valvular prosthesis surgery, immunosuppression, hemorrhagic fever, active malignant treatment, drug abuse, psychiatric disorders, as well as vascular bisphosphonate use.
What are limitations with dental implants?
The risks and complications of getting a dental vaccine include inflammation, other tooth damage, delayed bone healing, nerve damage, prolonged bleeding, jaw fractures and many more. If you are ready to take these risks, a dental vaccine may be right for you.
What are the contraindications for dental implant?
Complete challenges for dermatological rehabilitation include myocardial infarction and brain accidents, valvular prosthesis surgery, immune deficiency, bleeding issues, malignant active treatment, drug abuse, mental illness, as well as intravenous bisphosphonate use.
What are contraindications for bisphosphonates?
Contraindications to bisphosphonates include:
- Sensitive history of bisphosphonate.
- Hypocalcemia.
- Chronic kidney disease with glomerular filtration rate of less than 30 to 35 mL / min.
When do you give bisphosphonates for osteoporosis?
Infusion bisfosphonates (Ibandronic acid and Zoledronic acid) are recommended as the treatment for osteoporosis in adults if: o The person is eligible for a risk assessment, and o 10-year probability of osteoporotic fracture is at least 10%, OR o 10-year probability of osteoporotic fracture is …
What is an indication of alendronate?
Alendronate sodium tablets, USP is intended for the treatment of osteoporosis in postmenopausal women. In postmenopausal women, Alendronate sodium tablets, USP increases bone density and reduces the incidence of fractures, including those of the hip and spine (vertebral fractures).
Why are bisphosphonates contraindicated in dental implants?
All patients treated with bifosphonates should have a potential risk of bone loss and risk of developing bone marrow necrosis, and provide informed consent prior to dental surgery.
How does bisphosphonates affect dental treatment?
Although bisphosphonates have been shown to be beneficial for many bone marrow diseases, but because of their osteoclast action, they impair bone healing and remodeling this poses an increased risk of developing osteonecrosis of the jaw (ONJ ) After dental procedures such as extraction or implant. ..
How do bisphosphonates affect dental implant success?
Because bisphosphonates interfere with the function of osteoclasts it can increase bone density. Because new bones need bones to heal, the new bone around the new tooth enamel must be eaten by osteoclasts before new bones can form.
Should I stop taking Fosamax before tooth extraction?
Because Bisphosphonate remains in the bone for a long time even after discontinuation, it is not usually recommended for the patient to stop taking bisphosphonate before it is taken.
How long should you be away from Fosamax before a tooth extraction? These studies also suggest that stopping bisfosphonate 3 months before the procedure appears to reduce the incidence of osteonecrosis.
Should you stop Fosamax before dental work?
Some of these conditions are serious risk factors for osteoporosis. However, Sedghizadeh noted that USC is now warning all dental patients taking Fosamax and other bisfosphonates “you may be at risk of developing osteonecrosis (bone death) of the jaw, and some dental treatment may increase that risk. . “
Can you have dental work while taking alendronate?
Although the risk of osteonecrosis after dental surgery is low, many dentists recommend stopping the use of alendronate three months before the procedure if you have been taking the medication for more than three years.
When should I stop taking Fosamax before tooth extraction?
AJOMS staff on ONJ recommends discontinuation (drug clearance) of oral BPs for at least two months prior to the treatment of “at-risk” dental caries in patients with a long history of exposure (> 4 years), pathogenesis, or glucocorticoids or antiangiogenic drugs.
When should I stop taking alendronate before dental surgery?
AJOMS staff on ONJ recommends discontinuation (drug clearance) of oral BPs for at least two months prior to the treatment of “at-risk” dental caries in patients with a long history of exposure (> 4 years), pathogenesis, or glucocorticoids or antiangiogenic drugs.
When do you stop taking bisphosphonates before dental surgery?
The American Association of Oral and Maxillofacial Physicians does not object to dental placement in patients receiving oral bisfosphonates less than three years prior to surgery provided they do not present other serious issues such as steroids or premature aging.
Can I have a tooth extraction while taking alendronic acid?
If you have implanted teeth or runny teeth while taking alendronic acid, there is a very small chance of damage to the jaw bone. For safety, tell your dentist that you are taking alendronic acid. They may recommend a different type of dental treatment.
When can I stop using bisphosphonates before tooth extraction?
If systemic conditions allow, the physician may consider stopping oral bisfosphonates for three months before and three months after the selected dental surgery to reduce the risk of BRONJ.
When should bisphosphonates be stopped?
To reduce the risk of these rare complications, your doctor may recommend that you temporarily stop taking bifosphonates after 3 to 5 years. This is sometimes called bisphosphonate release. People with osteoporosis may need to wait 10 years before stopping taking these medications.
Can you have a tooth pulled while on Fosamax?
According to our data, dental extraction appears to be safer for osteoporosis patients treated with oral bifosphonates. Introduction: Oral bisfosphonates are drugs commonly prescribed for the treatment of osteoporosis and other resorptive bone diseases.
Do you gain weight with Fosamax?
Weight gain is not a risk factor for taking Fosamax. Clinical trials, weight gain did not occur in people taking Fosamax. However, chronic inflammation (swelling of your arms or legs) has been reported by some people since Fosamax was approved by the FDA and released on the market.
What are the most common side effects of Fosamax? The manufacturer of the drug, Merck, said the most common side effects include stomach issues, such as nausea, diarrhea, constipation and cramps.
What can you not take with Fosamax?
Calcium or minerals, vitamins, antacids, coffee, tea, soda, mineral water, calcium-rich juices, and foods can reduce alendronate absorption. Do not take these for at least 30 minutes (preferably 1 to 2 hours) after taking alendronate. Take this medicine regularly to get the most benefit from it.
What happens if you drink coffee after taking Fosamax?
Coffee can reduce the amount of alendronate (Fosamax) absorbed by the body. Taking coffee and alendronate (Fosamax) at the same time may reduce the effectiveness of alendronate (Fosamax). Do not drink coffee within two hours of taking alendronate (Fosamax).
What medications should not be taken with Fosamax?
Calcium Supplements / Antacids The combination of Fosamax administration and calcium, antacids, or oral medications including multivalent cations will interfere with Fosamax absorption. Therefore, tell patients to wait at least half an hour after taking Fosamax before taking other oral medications.
Should Fosamax be taken in the morning or at night?
It should be taken as soon as you get out of bed in the morning and at least 30 minutes before meals, drinks, or other medicines.
Why can’t you eat after taking Fosamax?
Foods and beverages (for example, mineral water, coffee, tea, or juice) will lower the amount of alendronate absorbed by the body. Waiting more than 30 minutes allows more of the medicine to be absorbed.
Why do you have to sit up after taking FOSAMAX?
Do not lie down after taking the medicine. Alendronate damages the esophagus and the water will wash the medicine down to the stomach. If you lie down the medicine may return to the esophagus, so you should not lie down.
Does FOSAMAX need to be taken on an empty stomach?
FOSAMAX is effective only when taken on an empty stomach. Staying upright allows the pill to settle quickly in your stomach and may help you avoid certain side effects such as heartburn, chest pain, or discomfort or pain when swallowing. If you have to lie down, wait 30 minutes, have breakfast, and then lie down.




Comments are closed.