Can i get a dental implant if i have diabetes
Who is not suitable for dental implants?
People who are taking certain medications, such as steroids or drugs that suppress the immune system, may also not be suitable candidates. On the same subject : Do you need dental implants. And people with certain habits, such as people who grind or grind their teeth heavily, can put too much pressure on the implants, causing long-term damage.
Is everyone suitable for dental implants? Can anyone get dental implants? In most cases, anyone can be healthy enough to undergo a routine tooth extraction or oral surgery for a dental implant. Patients should have healthy gums and enough bone to hold the implant. They must also engage in good oral hygiene and regular dental visits.
When are dental implants not possible?
To have implants placed, a patient must undergo oral surgery. So, the patient must be in good physical health. To see also : Dental Implant Clinic. They must also have adequate bone in the jaw to support the implants. If they have suffered from chronic diseases like diabetes or leukemia, they may not be a good candidate for dental implant surgery.
Why am I not suitable for dental implants?
Patients with systemic diseases such as diabetes, Parkinson’s disease and certain autoimmune diseases have a higher risk of infection or implant complications. Osteoporosis, medications used for osteoporosis and other bone deteriorating diseases, also contribute greatly to implantation complications.
Who cant have implants?
People with gingivitis, periodontitis or any other form of dental disease may not have dental implants. This is because this condition destroys the gums and bone underneath. This may interest you : Does dental insurance pay for implants and bridges. As a result, too much bone loss leads to a lack of enough bone to secure the implant. Dentists often suggest treating dental disease first.
What are limitations with dental implants?
The risks and complications you take for dental implants include infection, damage to other teeth, delayed bone healing, nerve damage, prolonged bleeding, jaw fractures and more. If you are willing to take these risks, dental implants may be right for you.
Who is not suitable for dental implant?
You may not be suitable for dental implant treatment if you have certain medical conditions. These include uncontrolled diabetes, blood clotting diseases, cancer, problems with the immune system and drug abuse.
How do I know if I’m allergic to titanium?
It is possible to detect a titanium allergy in advance with a MELISA test. This type of blood test isolates your white blood cells, exposes them to titanium and measures the immune response to titanium.
Can I be allergic to titanium piercing? Titanium particles are too large to penetrate the skin and the relationship between skin sensitivity and systemic hypersensitivity is poorly defined. The Mayo Clinic conducted a decade of patch testing and found no positive reactions to titanium despite published cases of titanium hypersensitivity.
Can your body have a reaction to titanium?
One of the causes of implant failure can be attributed to allergic reactions to titanium. There have been reports of hypersensitive reactions such as erythema, urticaria, eczema, swelling, pain, necrosis, and bone loss due to titanium dental implants [15, 67, 68].
Can you be allergic to medical titanium?
Titanium allergies are rare, occurring in about 0.6% of the population, according to a study. That means as many as 1.8 million people in the US may be allergic to titanium to some degree. Other studies suggest that the allergic reaction or hypersensitivity to titanium may be much higher.
How do you know if your body is rejecting titanium?
Seminal studies cited by the International Journal of Implant Dentistry report that titanium allergy symptoms include: Erythema (skin redness, in this case, in the tissue around the implant) Urticaria (yeasts that can be seen on the skin or gum surface) Eczema (itching) Inflammation of the skin or gums)
Can your body reject titanium implants?
Titanium implants integrate with your jawbone and are unlikely to be discarded unless you are accustomed to following habits that are detrimental to placements.
Do titanium implants fuse with bone?
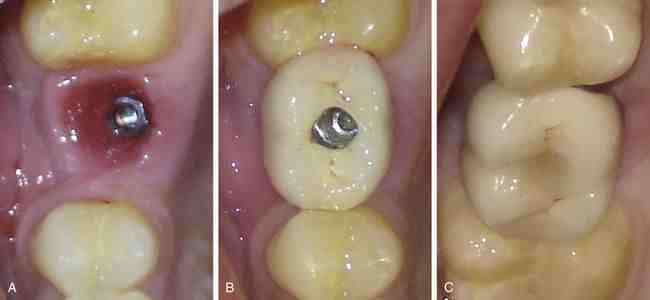
Titanium dental implants are those that are surgically implanted directly into the patient’s jaw. This allows the implant post to remain firmly anchored in place as the bone fuses over time. Essentially, a titanium implant mimics the function of a natural tooth root.
Will your body reject implants?
According to the International Congress of Oral Implantologists, it is rare for your body to reject your dental implants. However, this does not mean that your dental implant will not fall off. A successful dental implant is one that is placed in healthy bone and is properly cared for after the surgery takes place.
What are the symptoms of an allergic reaction to titanium?
Clinical Characteristics of Hypersensitivity to Titan. The researchers described several clinical manifestations in patients with titanium allergies, including episodes of hives, eczema, edema, redness and itching of the skin or mucous membranes, which may be localized or generalized.
How do you know if you are allergic to titanium?
Titanium Allergy Symptoms & Tests It is possible to detect a titanium allergy in advance with a MELISA test. This type of blood test isolates your white blood cells, exposes them to titanium and measures the immune response to titanium.
Are titanium allergies common?
Titanium allergies are rare, occurring in about 0.6% of the population, according to a study. That means as many as 1.8 million people in the US may be allergic to titanium to some degree. Other studies suggest that the allergic reaction or hypersensitivity to titanium may be much higher.
How long does it take for a diabetic to heal after tooth extraction?
Twenty-eight patients, 12 (5%) diabetics and 16 (7%) control group, had socket healing delayed for more than one week, but all healed within four weeks. There were no statistical differences between delayed healing and age, gender, diabetic state, BGL, or smoking.
How long does it take to close the hole after tooth extraction? Surgical Extraction Healing Time Your teeth hole will be completely or almost completely closed about 6 weeks after surgery. The indentation will usually fill up after a few more months and heal completely. Surgical extraction is often required to remove: it affects teeth, such as wisdom teeth, which do not erupt in your gums.
Do diabetics take longer to heal after tooth extraction?
Diabetes can reduce your resistance to infection and can slow down the healing process. If you have extensive oral surgery, your dentist may prescribe antibiotics to minimize the risk of infection. To help the healing process, keep your blood sugar level under control before, during and after surgery.
Are diabetics more prone to dry socket?
People with diabetes are more likely to develop dry socket. If you have a tooth or gum in the area of extraction, this can lead to dry socket. Most diseases do not increase the chances of having dry socket.
Can I have tooth extraction if I am diabetic?
People with diabetes need to be careful because extractions of the gums open up to an infection. This infection can cause hyperglycemia and mobilize fatty acids, leading to acidosis. All of these conditions make the control of blood sugar levels extremely difficult.
Are certain people prone to dry socket?
Women tend to have dry socket more often than men. In fact, according to the Academy of General Dentistry, women who take oral contraceptives are twice as likely to get dry socket due to elevated estrogen levels.
Can a diabetic person have tooth extraction?
But all said and done, diabetics who are aware of their blood sugar levels and take proper care to keep it under control can go for dental extraction safely after two weeks of medication.
Can diabetics get dentures?
Diabetics with controlled sugar levels have the same success rate of the area as a non-diabetic. Studies have found a direct correlation between those who have well-regulated sugar levels and those with good oral health. Making sure your dentures are clean and properly fitted will help reduce the risk of infection.
Do I need to tell my dentist Im diabetic?
Yes, it is important for your dentist to know that you have diabetes. If you are taking medication, tell your dentist the name and dosage of the medication. If you are having difficulty with blood sugar control, let your dentist know because poor glucose control can affect your teeth and gums.
What makes a good candidate for dental implants?
Most people are good candidates dental implants can replace one, some or all of your teeth. They can be used in place of bridges or dentures. Good candidates have healthy gums and are old enough to stop their gums from growing. You should also have enough bone to support and anchor the implants.
Why am I not suitable for dental implants? Patients with systemic diseases such as diabetes, Parkinson’s disease and certain autoimmune diseases have a higher risk of infection or implant complications. Osteoporosis, medications used for osteoporosis and other bone deteriorating diseases, also contribute greatly to implantation complications.
Who would be a candidate for dental implants?
Dental patients who do not make good candidates for all at 4 have a history of poor oral health and have subterranean conditions that make healing after implant surgery difficult or unusually slow.
What makes you a candidate for dental implants?
Prerequisites for Dental Implants You need to have a strong, healthy gums and gums for dental implants to be a viable dental replacement option for you. If you have experienced bone loss due to a dental cessation, or are suffering from oral health problems like gingivitis, dental implants may not be for you.
Who is not a candidate for dental implants?
But not everyone is a viable candidate for implants, and ironically the reason is mostly bone. If a patient has suffered a significant loss of bone volume, either due to disease or the long-term lack of natural teeth, there may not be enough bone to properly support an implant.
Is everyone a good candidate for dental implants?
But not everyone is a viable candidate for implants, and ironically the reason is mostly bone. If a patient has suffered a significant loss of bone volume, either due to disease or the long-term lack of natural teeth, there may not be enough bone to properly support an implant.
What is the failure rate of dental implants?
Dental implants have a high success rate, but some people experience dental implant failure. It is estimated that about 5 to 10 percent of dental implants fail, either shortly after a procedure or months or years later.
What makes a good candidate for dental implants?
The perfect candidate for an implant is in good oral health and general health. Adequate jawbone is necessary to support a dental implant, and the ideal candidates should have healthy tooth tissue free from periodontal disease. Implants are connected to underground bones and gum tissue in the mouth.
Can dental implants cause death?
This case shows that even simple implantological procedures, which are often considered routine and risk-free, lead to serious and potentially fatal complications.
Are dental implants lowering life expectancy? Tooth loss can shorten your life! Fortunately, however, dental implants can restore your smile and perhaps increase your lifespan.
Can dental implants cause a stroke?
NEW YORK (Reuters Health) – For people who have dental surgery, the risk of heart attack and stroke may increase in the weeks after the procedure, says British research. “This is the first sign of increased risk of heart attack or stroke after a dental procedure,” co-author Dr.
What are the risk factors associated with dental implants?
Possible risk factors before going to surgery and how to overcome these risks:
- Bacteria build up: Bacteria build up can pull back gums, and it makes the implant screws visible and also allows bacteria to cause an infection. …
- Infection and inflammation: …
- Rejection: …
- Captures the Nerve:
Can dental implants cause blood clots?
General instructions. After implantation, a blood clot may form in the area. To prevent postoperative inflammation and infection, it is important to keep this blood clot in place.
What are the most common problems with dental implants?
What are the risks of getting dental implants?
- Sinus damage: A major risk for dental implants is sinus damage. …
- Infection: Like any oral surgery procedure, dental implant surgery carries a risk of infection. …
- Nerve damage: It is possible for implant surgery to lead to nerve damage.
Can dental implants harm you?
Dental implant risks are rare, but they can occur just like with any other surgery. Such risks may include injury and infection at the implant site. Nerve damage and sinus problems can also occur, and the prompt intervention of your prosthodontist can be vital to recovery.
Do dental implants cause health problems?
What can go wrong? All oral surgeries involve a small risk of bleeding disorders, infections and allergic reactions. Fortunately, long-term complications – as the Mads suffer – occur on a rare basis. However, an implant that is placed too close to a nerve can cause numbness or tingling in the tongue, lips, gums or face.
Can dental implants cause problems years later?
But sometimes something will go wrong and patients will experience dental implant problems years later. Even if it does not happen often, it is a possibility. These issues can become major sources of stress for those patients who experience it.
Do diabetics need antibiotics for dental work?
If emergency surgery is needed for a poorly controlled patient, then prophylactic antibiotics should be taken with the accepted principles of such use. Infections in diabetic patients, regardless of their control levels, should be managed aggressively, including possible early referral to oral and maxillofacial surgeons.
What medical conditions require antibiotics before dental work? Antibiotics can be used in cases of an abscess or periodontal disease (gum infection). It is usually a necessary component of such procedures as tooth extraction, root canal therapy or deep cleaning of the gums. In other cases, antibiotics may be prescribed to prevent infection.
What dental procedures require antibiotic prophylaxis?
Procedures that require prophylaxis include:
- Teeth cleaning.
- Tooth extractions.
- Periodontal procedures when bleeding is predicted.
- Scaling and root planning.
- Reimplantation of avulsed teeth.
- Root canal treatment over the top.
- Initial placement of orthodontic bands (not brackets)
- Intraosseous or intraligamentary injections.
What dental procedures needs prophylaxis?
Antibiotic prophylaxis (or premedication) is simply the antibiotics before some dental procedures such as tooth cleaning, tooth extractions, root canals, and deep cleaning between the tooth root and gums to prevent infection.
Which clients will require prophylactic antibiotics before certain dental procedures?
Antibiotic prophylaxis is warranted for some patients with heart disease and compromised immunity when undergoing dental procedures that involve manipulation of the gingival tissue or the periapical region of the teeth or perforation of the oral mucosa.
Is there a need for antibiotic prophylaxis after routine dental extraction in diabetic patients?
We propose that the use of perioperative prophylactic antibiotics for routine extractions in controlled diabetic patients is not justified and does not provide evidence based on the same evidence as is not indicated in non-diabetic patients.
Do diabetics need prophylactic antibiotics?
For diabetic patients, intraoperative re-dose of prophylactic antibiotics may be an independent protective factor for SSI prevention. A specific perioperative antibiotic injection strategy should be encouraged for diabetics with prolonged surgery to minimize the possibility of SSI.
Which patient would require prophylactic antibiotics prior to dental procedure?
Prophylaxis against IE is reasonable prior to dental procedures involving manipulation of the gingival tissue, manipulation of the periapical region of the teeth, or perforation of the oral mucosa in patients with the following patients: homografts.
How does diabetes affect dental treatment?
Periodontitis tends to be more severe in people who have diabetes because diabetes has the ability to resist infection and slows healing. An infection like periodontitis can also raise your blood sugar level, making your diabetes more difficult to control.



Comments are closed.