How long before dental implants can i get steroid injection in back
Steroids are an anti-inflammatory. However, an inflammatory response is required in case of infection. It carries the white blood cells and antibodies needed to fight the infection.
How long does it take for bone to grow after dental bone graft?
How long does it take for the bone to heal after the grafting of the dental bone? Everyone’s mouth is unique, and there is no specific time frame for how long it takes for the bone graft to fuse with the natural bones that are already in the mouth. To see also : Bone Graft Healing Time. Generally, it can take anywhere from three months to a year for bone grafting to join.
How long does it take for the gum to grow on the bone graft? Unfortunately, your mouth is different from any other and there is no exact time frame for how quickly this happens. It is not uncommon to take three months to a whole year for bone grafting to fuse with natural bones in the mouth.
Can you feel a bone graft growing?
In general, you can expect to feel more normal after a few weeks. After your initial recovery, your bone graft needs time to heal and grow a new jaw. Read also : Dental Implant Pricing. You may not feel pain during this growth process, but you know it can take several months.
How do I know if my bone graft is coming out?
Severe Pain: While a certain level of pain is to be experienced, this pain should be relatively manageable with the help of pain medications that are typically prescribed by your oral surgeon. However, if this pain is severe and / or lasts for several days or weeks, this is a sign that your bone graft has probably failed.
What does a failed bone graft feel like?
Immediate alert signals are as follows; Draining of severe secretion from the area of surgery and intense pain, even after a few days of surgery. The area turns red, and there is no reduction in sugar. After surgery, the new bone attaches and grows into the gums.
Does bone grow back after bone graft?
Once the bone graft has been placed, hold the space for your own body to do the repair work. This may interest you : People With No Teeth. In other words, a dental bone graft is like a scaffold on which your own bone tissue can grow and regenerate.
How does bone grow after bone graft?
What happens after a bone graft procedure? Over time, the graft material develops into (fuse with) nearby bone tissue. This process can take anywhere from several weeks or up to a year. The duration of your recovery depends on the size and location of the bone graft.
Does bone graft last forever?
Also, the mineral graft materials that are used are naturally absorbed over the top and replaced with your own bone. This means that they will not stay in your body forever, so there is no cause for concern.
How long does it take for a dental bone graft to heal?
Recovery time after the procedure The time required for recovery will depend on the size of the bone graft or the defect being treated. Your recovery may take two weeks to 3 months, but the bone graft itself will take three months to heal.
How long does it take for gums to heal after a bone graft?
In the healing stages of bone grafting, the incision in your gums heals quickly – usually within a couple of weeks or so. Tooth extraction will take longer to heal the bone graft. The area where the grafting material is applied takes longer to return to normal – sometimes up to nine months.
How long does it take for dental bone graft to harden?
Maturation. The graft “matures,” or transforms into your own bone, over a period of 3-6 months. An appointment for implantation will be scheduled once your graft is mature. Vigorous reinforcement should be avoided for the first week so that the graft material is not washed out.
What antibiotics treat infected dental implants?
Although there are numerous antimicrobial agents available, only a limited number of systemic antibiotics such as amoxicillin; phenoxymethylpenicillin (PcV); clindamycin; metronidazole; and the combination of amoxicillin and metronidazole have been widely used in the field of dental implants (Table 1).
How to treat an infected dental implant? Depending on the level of infection, your dentist may prescribe special mouthwashes or present a combination of other options to get your implant back on track. Treatment options may include antibiotics, surgery, laser therapy with surface decontamination, mechanical debridement, or antimicrobial therapy.
Can antibiotics clear up a dental implant infection?
4. Route of antibiotic delivery with dental implants. The use of oral antibiotics is one of the most common approaches in the treatment of bacterial infections. Antibiotics can be sent both systemically and by direct placement in the pouch around the dental implant.
Can dental implant infection be treated with antibiotics?
The use of oral antibiotics is one of the most common approaches in the treatment of bacterial infections. Antibiotics can be sent both systemically and by direct placement in the pouch around the dental implant.
Can you save an infected dental implant?
In most cases, peri-implant mucositis is highly treatable and reversible. That’s why you should see your dentist as soon as possible if you notice that the gums around an implant are red, bleeding or swollen.
What happens if dental implant gets infected?
When the infection attacks the bone, the bone begins to deteriorate. Thus, the implant loses its support base and may begin to feel loose. In severe cases, the infection can sneak into the bloodstream and cause systemic health problems. Surgery is usually necessary to deal with peri-implantitis.
What happens if an implant becomes infected?
An infected implant can lead to a systemic disease that can cause damage to the heart and other organs of the body. If not treated long enough, low quality bacterial infections can have serious consequences and have the potential to become very dysfunctional very quickly. Your dentist wants you to be healthy.
Can an infected dental implant be saved?
In most cases, peri-implant mucositis is highly treatable and reversible. That’s why you should see your dentist as soon as possible if you notice that the gums around an implant are red, bleeding or swollen.
Do I need antibiotics for dental implant?
Prophylactic antibiotics for any implant surgery are not required. However, antibiotics are useful for the prevention of postoperative infections after implantation. To achieve long-term survival and a successful rate of dental implants, antibiotic prophylaxis is necessary.
What antibiotic is best for dental implant infection?
The most common first-line drug was amoxicillin, with amoxicillin-clavulanic acid as the second choice. Conclusions: The majority of dentists from different countries do not prescribe systemic antibiotic prophylaxis for dental implant surgery following the available scientific evidence and could be overprescribing.
Do you need antibiotics before dental implant?
Navid Rahmani might suggest the use of antibiotics, possibly before dental implant surgery. It could be particularly important if you have a higher risk of developing an infection. The use of antibiotics before surgery will help prevent bacteria from infecting your body.
What medications can cause dental implants to fail?
This includes popular antidepressants such as fluoxetine (Prozac), sertraline (Zoloft) and paroxetine (Paxil). These medications can interfere with your body’s ability to integrate the implant into the bone. Studies vary how big the risk is. Some say that SSRIs double your risk of implant failure.
What could be the reason that implants could fail? Implants can fail for a number of reasons, including integration failure, implant fractures, implant malpositions that cause damage to vital structures (such as the lower alveolar nerve, sinus membrane, a natural tooth, or an adjacent implant), and advanced bone loss. around an integrated, loaded implant, which results in …
What can affect dental implants?
Medications that can interfere with the healing of the dental implant
- Antidepressants. One of the medications with the highest risk profile for dental implants is selective serotonin reuptake inhibitors (SSRIs). …
- Painkillers. …
- Dressings for osteoporosis. …
- Other prescription drugs. …
- Recreational drugs. …
- Considering dental implants in Anchorage?
Do dental implants deteriorate?
An implant will never decay or need root canal treatment, and it feels like the tooth that was there. Replace multiple teeth – When you have more than one missing tooth, implants provide an ideal replacement mechanism.
What are the signs of dental implant failure?
While there are many different possible causes of implant failure, the signs are the same. You know that your dental implants will fail if you start to experience severe pain or discomfort in or around your dental implants, if your gums are swollen or inflamed, or if your implant starts to come loose.
What is the most common cause of implant failure?
Dental implants can fail for a variety of reasons, but the most common – and most preventable – are infection and bone loss. Peri-implantitis is a type of infection that forms around the implant and inside the gums.
What causes early dental implant failure?
Lack of primary stability, surgical trauma, and infection appear to be the leading causes of initial implant failure. The first signs of infection may be an indication of a much more critical outcome than if the same complications occurred later, due to disruption of the primary process of bone healing.
How common is it for an implant to fail?
Dental implants have a high success rate, but some people experience dental implant failure. It is estimated that about 5 to 10 percent of dental implants fail, either shortly after a procedure or months or years later.
Why do doctors prescribe steroids after surgery?
The literature indicates that the use of a steroid is a safe and effective way to reduce postoperative pain and edema. Studies have shown that steroids delay healing, inhibit collagen synthesis and increase the risk of postoperative infection.
Why does a doctor give a patient steroids? Corticosteroids are used to treat rheumatoid arthritis, inflammatory bowel disease (IBD), asthma, allergies and many other conditions. These drugs also help suppress the immune system to prevent organ rejection in transplant recipients.
Do steroids speed up healing?
Anabolic steroids can help in the healing of muscle contusion injury by accelerating the recovery of strength generation capacity.
Why do steroids affect wound healing?
Steroids have also been shown to affect long-term wound healing. Doses of steroids greater than 30 mg / day inhibit the activity of fibroblasts and therefore prevent tissue contraction, as well as scar reduction and shortening.
How do steroids help heal the body?
Steroids work by reducing inflammation and reducing the activity of the immune system. Inflammation is a process in which white blood cells and body chemicals can protect you from infection and foreign substances such as bacteria and viruses.
What steroids are given after surgery?
During surgery, dexamethasone is given to the patient to reduce the risk of nausea and vomiting after surgery, to relieve pain, and to make the patient feel better.
How do steroids affect healing?
Glucocorticoids (corticosteroids) cause dehiscence of surgical incisions, increased risk of wound infection, and delayed healing of open wounds.
Do steroids reduce healing?
Steroids have also been shown to affect long-term wound healing. Doses of steroids greater than 30 mg / day inhibit the activity of fibroblasts and therefore prevent tissue contraction, as well as scar reduction and shortening.
Do steroids speed up wound healing?
While the use of high-dose acute systemic corticosteroids is unlikely to have a clinically significant effect on wound healing, chronic systemic corticosteroids may prevent postoperative healing in susceptible patients.
How long should I take antibiotics after dental implant?
The risk of infection is high. Implant surgery with floor sinus lifting, autogenous block bone grafting, and the same procedures as category 2 and 3, but on medically compromised patients. The suggested regimen is like category three, but postoperative antibiotics are recommended for 5 days.
What is the best antibiotic for dental implant infection? The most common first-line drug was amoxicillin, with amoxicillin-clavulanic acid as the second choice. Conclusions: The majority of dentists from different countries do not prescribe systemic antibiotic prophylaxis for dental implant surgery following the available scientific evidence and could be overprescribing.
How long should you take antibiotics for after oral surgery?
Antibiotics will be given to help prevent infection. If you are prescribed Amoxicillin 500mg, take 1 capsule every 8 hours for seven days or otherwise as prescribed by your doctor.
How often do I take antibiotics after wisdom teeth removal?
You will usually also be given an antibiotic to take a week after your procedure. For your initial dose, start taking two pills and then one pill 4 times a day (after breakfast, lunch and dinner, and before bed). NAUSEA: Nausea is not uncommon after surgery. Sometimes pain medications are the cause.
Should you take antibiotics after oral surgery?
Every patient has an oral bacterium that could cause an infection if it gets into their bloodstream. For most healthy patients, their immune system protects them from such an occurrence and antibiotics are prescribed only after dental surgery if an infection is found as a complication.
How common is infection after dental implant?
The good news is that the risk of infection after dental implant surgery is relatively low, and even treating the infection can be easy if a patient sees a dentist after developing warning signs. Symptoms of infection include the following: Red or swollen gums at the implant site. Loose or shaky implants.
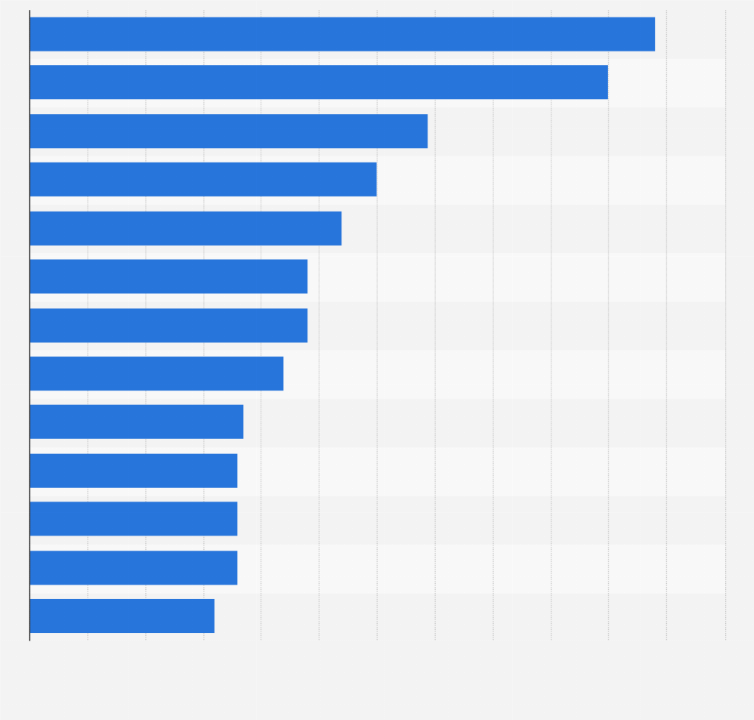
What percentage of dental implants become infected?
Four to 10% of patients receiving dental implants develop postoperative infections. This complication is important because the treatments applied are generally ineffective, and two-thirds of the infected implants fail, most prior to prosthetic loading.
How can I prevent infection after dental implant?
Avoiding infection
- Rinse mouth with salt water. While this is not recommended during the first day of your recovery, rinsing your mouth with salt water for the rest of your recovery can help control the bacteria while your wound heals.
- I don’t smoke. …
- Keep brushing. …
- Switch to a sweet diet.
Should you take antibiotics after tooth implant?
Antibiotics – Patients should take all prescribed antibiotics to prevent infection at the surgical site. Twenty-four hours after surgery, patients should start using the prescribed oral rinse twice a day alongside a hot salt water rinse 4-5 times a day (preferably after each meal / snack).
Do I need antibiotics after dental implant?
Prophylactic antibiotics for any implant surgery are not required. However, antibiotics are useful for the prevention of postoperative infections after implantation. To achieve long-term survival and a successful rate of dental implants, antibiotic prophylaxis is necessary.
Are infections common with dental implants?
Dental implants are a useful and relatively common dental procedure. About 500,000 people undergo these procedures each year in the United States, more than half of which occur in the office of a general dentist. Although most implants come in smoothly, rare complications such as infections are possible.



Comments are closed.