How to get rid of dental implant infection
Peri-implantitis is usually the result of incorrect maintenance and oral hygiene habits. However, failed implants can be treated and restored.
Can peri-implantitis be reversed?
Fortunately, peri-implantitis can be successfully reversed and the health of your dental implants and smile restored with specialized treatment by our oral surgeons.
Can an infected dental implant be saved? Can an infected dental implant be saved? The sooner the infection is treated, the better the chances of success. On the same subject : What is the average cost of dental implants in florida. If a dental implant is already removed due to a severe infection and subsequent bone loss, it may not be possible to save it.
How serious is peri-implantitis?
In the early stages of peri-implantitis, the symptoms are relatively mild. Most experience swollen gums, leading to tenderness and sensitivity in the mouth. This may interest you : How much do mini dental implants cost. The longer the infection is left untreated, the more serious the side effects will become.
How quickly does peri-implantitis develop?
Current studies indicate that 20% of implants develop peri-implantitis 6-7 years after placement. More recent studies suggest that the risk may be even higher and find that the occurrence of peri-implantitis increases with an increasing number of years that an implant is in service.
Is peri-implantitis an emergency?
A dental implant emergency can be defined as any situation that compromises the function of an implant and endangers its long-term viability. Two of the most common types of dental implant emergencies are: Peri-implantitis.
What happens if peri-implantitis is left untreated?
Peri-implantitis if not treated can progress to the severe stage and eventually lead to the loss of the implant. See the article : Dentchers. If caught early, and with proper supervision by a competent dentist, peri-implantitis can be treated before it ever causes undue discomfort or embarrassment.
Is peri-implantitis an emergency?
A dental implant emergency can be defined as any situation that compromises the function of an implant and endangers its long-term viability. Two of the most common types of dental implant emergencies are: Peri-implantitis.
Can peri-implantitis make you sick?
Peri-implantitis can be destructive and aggressive. An infected implant can lead to a systemic disease that can cause damage to the heart and other organs of the body. If it is not treated long enough, low grade bacterial infections can have serious consequences and have the potential to become very unfun very fast.
How long does it take to develop peri-implantitis?
Current studies indicate that 20% of implants develop peri-implantitis 6-7 years after placement. More recent studies suggest that the risk may be even higher and find that the occurrence of peri-implantitis increases with an increasing number of years that an implant is in service.
How often does peri-implantitis occur?
The current meta-analysis estimated the prevalence of similar peri-implantitis to be 12.8% at the implant level and 18.5% at the patient level.
How do I know if I have peri-implantitis?
What are the symptoms? Advanced peri-implantitis presents severe symptoms, but at first, you may not notice. Look at the bleeding, tender, red gum around the implant. In some cases, you may not notice tenderness or bleeding unless you apply pressure to the gums, such as by flossing or brushing.
Can dental implant infection be treated with antibiotics?
The use of oral antibiotics is one of the most common approaches in the treatment of bacterial infections. Antibiotics can be delivered systemically or by direct placement into the pocket around the dental implant.
How do you tell if a dental implant is infected? 5 Signs you have a tooth infection
- Pain and difficulty chewing. Having some pain is normal after any invasive dental procedure. …
- Fever, Redness, and Swelling. …
- The constant taste in the mouth. …
- Bloody pus or discharge. …
- Loose plants.
Can antibiotics clear up a dental implant infection?
The use of antibiotics with dental implant infection Antibiotics can be effective for prevention and for postoperative infections and can actually help the implant stay healthy in the long term.
Can infected dental implant be saved?
In most cases, peri-implant mucositis is highly treatable and reversible. This is why you should see your dentist as soon as possible if you notice that the gums around an implant are red, bleeding or swollen.
What antibiotic is best for dental implant infection?
The most frequent first-choice drug was amoxicillin, with amoxicillin-clavulanic acid as the second choice. Conclusion: The majority of dentists from different countries do not prescribe systemic antibiotic prophylaxis for dental implant surgery following the available scientific evidence and could be overprescribing.
What happens if my dental implant gets infected?
When the infection attacks the bone, the bone begins to deteriorate. Thus, the implant loses its base of support and can begin to feel loose. In severe cases, the infection can sneak into the bloodstream and cause systemic health problems. Surgical intervention is usually required to address peri-implantitis.
What antibiotics treat infected dental implants?
Although there are numerous antimicrobial agents available, only a limited number of systemic antibiotics such as amoxicillin; phenoxymethylpenicillin (PcV); clindamycin; metronidazole; and the combination of amoxicillin and metronidazole have been widely used in the field of dental implantology (Table 1).
What to do if a dental implant becomes infected?
If you suspect that you have an infected dental implant infection, it is very important to seek the help of a dentist. The infection will not get better by waiting and seeing if it goes away. Instead, you need to see a dentist as soon as you suspect an infection.
How is a dental implant infection treated?
Treatment options may include antibiotics, ultrasonic cleaning with surface decontamination, surgery, mechanical debridement and in case of significant bone loss, removal of the dental implant itself.
How do you fix an infected dental implant?
Depending on the level of infection, your dentist may prescribe special mouthwashes or present a combination of other options to get your implant back on a healthy track. Treatment options may include antibiotics, surgery, laser therapy with surface decontamination, mechanical debridement, or antimicrobial therapy.
Can dental implant infection be cured?
In most cases, peri-implant mucositis is highly treatable and reversible. This is why you should see your dentist as soon as possible if you notice that the gums around an implant are red, bleeding or swollen.
Is dental implant removal painful?
Is dental implant removal painful? No! Removing a failed dental implant is typically a painless procedure. You will likely be under local anesthesia and dental sedation while your dentist works to remove your failed implant.
How are failed dental implants removed? One method involves the use of a cutting device, called a milling cutter. This tool is designed to safely and precisely cut a small portion of your bone (0.5 to 1.0 mm) along the edge of the implant, which will release the tension on the implant and speed up its removal. .
How long does pain last after dental implant removal?
This is typically 3-4 days after extraction. Symptoms include a throbbing, radiating pain along the jaw. This condition will resolve without treatment, however, the pain can be managed with the use of analgesics and / or with medicated paste placed in the extraction site.
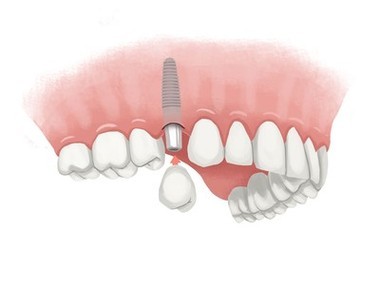
Why would a dental implant need to be removed?
Removal of the dental implant is rarely necessary. But when it is necessary, it is usually due to infections, inflammation or failure of the implant to integrate with the surrounding bone.
Do dental implants have to be removed?
When a dental implant fails, it is essential to remove it and possibly replace it before more serious problems occur. The affected area is repaired once the implants have been removed. If there is still enough healthy bone tissue on top, a new dental implant can be installed.
What happens if a dental implant has to be removed?
When removing a failed implant, your dentist aims to preserve as much healthy bone as possible. They may use a special tool called a bur to cut a small part of your bone (0.5 to 1.0 mm) along the edge of the implant.
What happens when an implant is removed?
After the removal of the implant, your breasts may droop, lower or appear misshapen. Many people choose to remove the implant with a breast lift (mastopexy). During a breast lift, your surgeon removes excess skin and reshapes the breast tissue. If necessary, the surgeon can also reposition the nipple and areola.
What to expect after removing implants?
In general, you should feel completely normal after getting your implant. Your arm may feel tender or swollen around where the implant was for a few days. It may look bruised for a week or two. Your doctor or nurse will tell you how to wash and care for your skin for a couple of days after removal.
Can you remove implants and not replace them?
If the implants are removed without replacement, there is often a volume of the breast and the discrepancy of the skin that cause drooping of the breast or aptosis.â Due to this fact, for those who are interested in the removal of the breast implant without replacement, her breasts may not be the same. as they did before undergoing breast augmentation.
Can a dental implant get infected years later?
Implant infections are caused by bacteria and can occur immediately after implantation or months or even years later. Also, if your dentist has not used titanium dental implants, an infection can develop due to the poor quality of the implant material used.
Why does my dental implant hurt years later? Did the pain start a year or more after dental implant surgery? Pain that begins a year or more after the procedure could be caused by closed or grinding teeth, problems with your dental hygiene, heavy smoking, an infection or inadequate bone.
Can your body reject a tooth implant years later?
When your body rejects an implant after the jaw bone has fully healed, it is categorized as late implant rejection. This can happen due to poor post-operative care, poor oral hygiene or trauma. Late rejection is typical about a year after implant surgery.
How do I know if my body is rejecting my dental implant?
This is when the body rejects an implant. Signs of rejection include increased pain at the site of implantation, swelling, fever and chills. A dental implant placed in the upper jaw can protrude into the sinus cavity. Injury to the area surrounding a dental implant can loosen the implant, resulting in failure.
Can dental implants failure years later?
Choosing an experienced and experienced dentist can eliminate some factors that impact dental implants. Late dental failure can occur 1 to 10 years after your surgery and can include: Bacterial infections. Extreme stress on implants.
How many years do dental implants last?
As mentioned above, dental implants last an average of 25 years. There are many reasons why implants can last less or longer than this average life. These reasons are discussed below. People with good oral hygiene will have their implants last longer.
How often should dental implants be replaced?
When maintained with proper hygiene and check-ups, dental implants can last a lifetime. The crown attached to the implant will usually be replaced every 15 to 20 years, although it can last several decades in some cases.
How long do full mouth implants last?
Life expectancy of full mouth implants The interval for normal wear and tear will be approximately 15 years. This depends on your diet, oral hygiene and other habits. Regular checkups monitor the condition of the crowns in the bridges.
Why is my gum sore around my implant?
Dental implants should provide adequate clearance for the gum tissue. If you don’t give enough space for your gums, it can lead to irritation or sore gums. Dental crowns can also irritate you if they don’t fit well with your other teeth.
Why does the gum around my implant hurt? Peri-implantitis is an infection that hurts the gums, bones and other tissues surrounding the dental implants. It is very similar to gum disease. The severity can vary from minor inflammation of the gums to severe degradation of the teeth and jaw.
How do you treat an infected gum implant?
Treatment options may include antibiotics, surgery, laser therapy with surface decontamination, mechanical debridement, or antimicrobial therapy. Your dentist wants you to be healthy. If you suspect an infected implant, contact a dentist immediately so that appropriate treatment can be started sooner rather than later.
What happens if my dental implant gets infected?
Peri-implantitis, an infection around dental implants, is an unfortunate possibility that, if left untreated, can become serious and result in removed implants, bone damage and/or gum complications.
Can infected dental implant be saved?
In most cases, peri-implant mucositis is highly treatable and reversible. This is why you should see your dentist as soon as possible if you notice that the gums around an implant are red, bleeding or swollen.
How do I know if my dental implant is failing?
You will know that your dental implants are failing if you begin to experience severe pain or discomfort in or around your dental implants, if your gums are swollen or inflamed, or if your implant begins to loosen. Treatment for failed implants depends on the cause of the failure.
Can a dentist tell if an implant is failing?
An implant that has failed will still be movable. Other signs of a dental implant that has lost osseointegration may include pain, swelling or infection, but this is not always the case. If your dentist notices that your implant is mobile, they may recommend an x-ray to check bone growth.
What are the signs of dental implant failure?
Late dental implant failure and problems Signs of damage include numbness or tingling in the tongue, lips, gums, or face. The rejection of the foreign body does not happen often, but it can happen. This is when the body rejects an implant. Signs of rejection include increased pain at the site of implantation, swelling, fever and chills.
How common is infection after dental implant?
Conclusion: Four to 10% of patients receiving dental implants develop postoperative infections. This complication is important because the treatments applied are generally ineffective and two thirds of the infected implants fail, most before the prosthetic load.
How do I know if my dental implant site is infected? Symptoms of dental implant infection include gums that bleed easily when brushing, tender or swollen gums around the implant and increased pocket depth around the implant.
Can dental implant infection be cured?
You may need a combination of different options to revive your implant, depending on the level of infection. A variety of treatments are available, including antibiotics, surgery, laser therapy with surface decontamination, mechanical debridement, and antimicrobial therapy. Healthy teeth are your dentist’s goal.
How do you get rid of an infected dental implant?
Treatment options may include antibiotics, surgery, laser therapy with surface decontamination, mechanical debridement, or antimicrobial therapy. Your dentist wants you to be healthy. If you suspect an infected implant, contact a dentist immediately so that appropriate treatment can be started sooner rather than later.
What happens when a dental implant gets infected?
Fever, Redness, and Swelling Like pain, some swelling around the surgery site is normal after getting dental implants. However, it should go down after the first few days. Increased swelling and redness, especially when accompanied by fever, is a symptom of infection.
How can I prevent infection after dental implant?
Good oral hygiene A robust oral hygiene routine is a recommended way to prevent infection after dental implant surgery. An implant patient’s oral hygiene routine should consist of brushing gently twice a day as normal. Regular brushing helps prevent the build-up of infection-causing bacteria.
What causes a dental implant to get infected?
An infection around a dental implant is a form of gum disease known as peri-implantitis. The infection can be the result of tobacco smoking, a failed oral hygiene routine, diabetes, a compromised immune system, bite misalignment, parafunctional habits (bruxism), or an allergic reaction to the implant itself.
Do I need antibiotics after dental implant?
Antibiotic prophylaxis for any implant surgery is not mandatory. However, antibiotics are useful for the prevention of postoperative infections after implantation. To achieve a long-term survival and success rate of the dental implant, antibiotic prophylaxis is necessary.
Are dental implant infections common?
Dental implants are a useful and relatively common dental procedure. About 500,000 people have these procedures each year in the United States, more than half of which occur in the office of a general dentist. Although most implants go in smoothly, rare complications such as infections are possible.
How do you stop dental implants from getting infected?
Maintain your oral hygiene. It is best to brush your teeth at least twice a day and floss every night before going to bed. Pay extra attention when cleaning your abutments and implants to remove trapped biofilm. Some people find it easier to use a waterflosser to clean difficult areas.
Are dental implant infections rare?
While relatively rare, dental implant infections can lead to implant failure and damage to the surrounding jawbone. But, with a few preventive measures and the right care and maintenance, you can greatly reduce the risk of infection.




Comments are closed.